Healthcare Cost Crisis- Reform Needs a “Triple A” Approach
by Kevin Power
Reformers should begin with an honest discussion of costs. A recent study in the Journal of the American Medical Association estimates 20-25 percent (or $760-935 billion) of American healthcare spending is wasteful3. This equates to annual government spending on Medicare and exceeds the Pentagon’s budget. The study suggests more competition or price controls (common in other countries) could reduce that amount by as much as one-third. Additional savings could flow by reducing administrative costs, currently in excess of $260 billion.
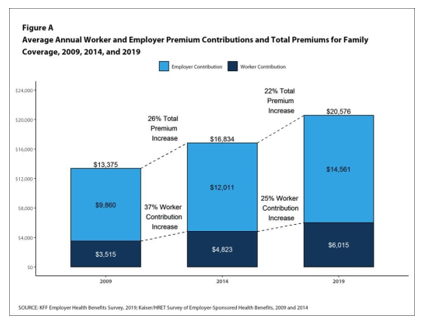
We should also acknowledge who pays for healthcare. Every employee, taxpayer, and consumer-
-no matter their health insurance program–assumes a share of the nation’s total healthcare costs. According to the Kaiser Family Foundation, the average total cost of employer-provided insurance for a family is $20,576 in 2019, a 50 percent increase since 2009.
1 Centers for Medicare and Medicaid Services, NHE Fact Sheet, 2017
2 CIA World Factbook
3 Waste in the US Health Care System, Estimated Costs and Potential for Savings, JAMA, October 7, 2019
The employer’s share is $14,561, and the employee’s share is $6,015 (with an average annual deductible of at least $1,600.) But “employer-provided” health insurance is not a “gift” to the employee; it’s part of his/her total compensation package. Add the employee’s contribution toward Medicare and Medicaid, plus state and local taxes (covering, for example, emergency room costs for the uninsured), and it’s clear that taxpayers bear the lion’s share of U.S. healthcare costs.
For years, corporations and insurance companies have been shifting costs to consumers in the form of higher premiums, deductibles, and prescription co-pays. However, the opaque nature of service pricing and the wildly different insurance coverage models leaves consumers confused and vulnerable. In our market economy, it would be difficult to identify another good or service where the consumer knows so little (or nothing) about the price before their purchase.
To rein in costs, consumers need the tools to manage their healthcare information and make informed decisions. The Economic Stimulus Act of 2008 provided $36 billion in taxpayer funds for healthcare providers to adopt electronic medical records (EMR), but these funds were distributed with few strings attached. A decade later, many providers have installed proprietary systems designed by IT specialists mainly to facilitate billing. But what about the patient? In a Deloitte Health study, 55 percent of patients reported their medical history was missing or incomplete when they visited their doctor. A Kaiser Family Foundation study found that 1 in 5 patients who were able to review their medical information discovered errors in their medical history.
While the healthcare industry touts “patient engagement” as its Holy Grail, in fact, current EMR systems are unnecessarily complicated, lack universal standards, and offer no financial incentives for providers to share information. So-called “patient portals” are frequently incomplete, difficult to access, and limited to the records of that particular practice. If you are treated by multiple providers, your information is likely scattered among disconnected, incompatible systems. In one high-profile case, the wife of a corporate executive had to bring printed copies of her medical records to every specialist she saw, because this information couldn’t be shared electronically. Her records were spread among more than 20 different EMR systems. Sadly, her experience is commonplace. If the provider has an EMR system, the patient or caregiver should be able to log on, and view and download information in a usable format.
Moreover, many providers refuse to accept anything other than a signed fax form (or an original signed form) rather than a request via secure electronic signature. In a wired mobile economy, this status quo must change.
A three-pronged, or ”Triple A” approach, would empower consumers to become active players in their own healthcare and help take control of their healthcare expenditures.
The first approach involves “access.” While industry grapples with the problem of information sharing between different EMR systems, the Federal government should enforce current regulations and should compel all providers to provide basic customer-facing improvements to help alleviate some of the pain in patient interaction with health providers. All patients have the right to receive medical information in an electronic format, where the provider has an EMR system. Under the ESIGN Act of 2000, electronic signatures and records have legal standing and healthcare companies already use this technology in their normal course of
business. Extending that practice to patients does not impose an additional burden on the provider, and may help reduce administrative costs. Release of Information forms for records should be acceptable if signed in person, sent via email, or through an electronic signature service. Electronic access to health information should be as easy as online banking.
The second approach involves “applications.” The market for consumer-friendly health management applications is underserved because patients find it difficult to obtain their health information. If access to their health information were readily available, developers would provide and consumers would use intuitive modern software applications to centralize their records and share with providers on a timely basis. Best practices routinely used for the provision of online banking, bill payment, and secure e-commerce can be applied to personal health information. Providing an easy way for patients to access, download, and disseminate their own records among different providers is an essential step toward achieving better outcomes and potentially lowering costs.
The last component of the “Triple A” approach involves “advocacy.” The road to more transparency in healthcare will require a sustained legislative and regulatory effort. For example:
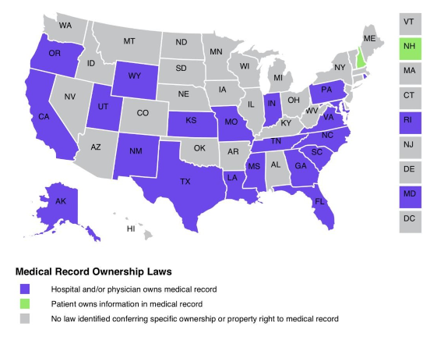
- Federal legislation is required to clearly establish ownership of the information in health records, replacing the existing patchwork of state laws. According to HeathInfoLaw.org Several large states, including California, grant ownership of medical records to the healthcare 4
4 Health Information and the Law- A project of the George Washington University’s Hirsh Health Law and Policy Program and the Robert Wood Johnson Foundation
In other states, while the patient may not own the medical record, they have legal ownership of the information in the record. A large number of states are silent on both counts. A uniform legal framework would eliminate ambiguity and establish an undisputed legal right to ownership of personal health data and the need to obtain explicit patient “consent” for the use of personal health data. This may help prevent future abuses like the recent discovery that Google and its healthcare partner Ascension compiled healthcare data on “tens of millions” of patients without their consent.
- Providers should be compelled to publish prices for standard treatments in a format that is readily accessible and understood by the general public, rather than attached to undecipherable billing
- Out-of-network charges without prior patient authorization should be eliminated. Insurance companies typically specify which providers are in-network and hence covered under their But the consumer is not protected from surprise bills from a hospital or practice that consults with an out-of-network specialist or practitioner. Responsibility for ensuring that approved covered treatments do not contain unanticipated out-of-network charges should be shifted from the consumers to the insurers and providers.
A “Triple A” approach is not a comprehensive solution to our healthcare dilemma, but it must be part of any effective reform.
Kevin Power is the Founder and Chairman of The Good Health Group, which provides health management tools to enable consumers to more effectively manage their health information. He has more than 30 years of operating and Board of Director experience in telecom, IT, and software with both public and private companies. He was Senior Advisor to the CEO and Board of Broadsoft, a NASDAQ listed company providing enterprise-focused unified communications services to telecom service providers. He was also Senior Advisor to the Global eHealth Foundation, chaired by Desmond Tutu.
Become an active health consumer! Start by downloading our free HealthEI app at: http://www.thegoodhealthnetwork.com/en/resources/products/healthei-app
and share it with family and friends via email, WhatsApp, Facebook and Twitter.